What Is the Difference Between FSAs and HSAs

HR Question:
We’ve been fielding a lot of benefits questions from our employees and some are trying to choose between opting into an FSA or HSA. What’s a good way to describe the difference between FSAs and HSAs?
HR Answer:
HR professionals play an important role in helping employees understand their benefits options so they can make the best decisions for themselves and their families. When it comes to managing healthcare expenses, it’s important for employees to be aware of the various options available to them. Two popular options are Flexible Spending Accounts (FSAs) and Health Savings Accounts (HSAs). Both accounts are designed to help individuals and families save money for medical expenses, but they have distinct features and eligibility criteria.
What are Flexible Spending Accounts (FSAs)?
A Flexible Spending Account (FSA) is a type of tax-advantaged savings account offered by many employers as part of their benefits package. FSAs allow an employee to set aside pre-tax dollars from their paycheck to cover eligible medical expenses. These expenses can include medical, dental, and vision costs that are not covered by their health insurance plan, such as co-payments, deductibles, prescription medications, and certain over-the-counter items.
One important characteristic of FSAs is the “use-it-or-lose-it” rule. This means that any funds contributed to an FSA must be used within the plan year, or the employee risks forfeiting the unused balance. Some plans offer a grace period or a limited rollover option, but these rules can vary, so be sure to explain your specific plan options.
Using FSAs for Dependent Care:
One noteworthy advantage of FSAs is their potential use for dependent care expenses, including childcare. If your organization offers a dependent care FSA, employees can contribute pre-tax dollars to cover eligible expenses related to the care of their children, disabled spouse, or elderly relatives who require care while they work or attend school. Eligible childcare expenses can include daycare services, after-school programs, summer day camps, and more. This feature can provide valuable financial relief for families with young children or dependents requiring care.
What are Health Savings Accounts (HSAs)?
A Health Savings Account (HSA) is another type of tax-advantaged account designed to help individuals save for qualified medical expenses. HSAs are typically paired with high-deductible health insurance plans. To be eligible for an HSA, the employee must be enrolled in a high-deductible health plan (HDHP) and cannot be covered by other health insurance, such as Medicare or another non-HDHP plan.
One significant advantage of HSAs is that the funds contributed are not subject to federal income tax, and they can grow tax-free over time. Unlike FSAs, there is no “use-it-or-lose-it” rule for HSAs. Any unused funds in an HSA can be carried over from year to year, allowing the employee to build up savings for future medical expenses or even retirement.
5 Key Differences Between FSAs and HSAs:
1. Eligibility
- FSAs: Generally available to employees regardless of their health insurance plan.
- HSAs: Available only to individuals with a qualified high-deductible health plan (HDHP).
2. Contribution Limits
- FSAs: The IRS sets annual contribution limits, and these limits can vary from year to year. The FSA contribution limits for 2023 are $3,050 with a maximum allowable carryover amount of $610.
- HSAs: The IRS also sets contribution limits for HSAs, and these limits are generally higher than those for FSAs. The limits may vary based on whether the employee has individual or family coverage. The HSA contribution limits for 2023 are $3,850 for self-only coverage and $7,750 for family coverage. Those 55 and older can contribute an additional $1,000 as a catch-up contribution.
3. Tax Treatment
- FSAs: Contributions are made with pre-tax dollars, reducing the employee’s taxable income.
- HSAs: Contributions are made with pre-tax dollars and can be invested, with earnings growing tax-free. Withdrawals for qualified medical expenses are also tax-free.
4. Rolling Over Funds
- FSAs: Typically have a “use-it-or-lose-it” rule, with limited exceptions for grace periods or rollovers. You should clarify your plan options to ensure your employees are correctly informed.
- HSAs: Funds can be carried over from year to year, and they remain available even if you change employers or health insurance plans.
5. Ownership
- FSAs: Generally owned by the employer, though employees can use the funds for eligible expenses.
- HSAs: Owned by the individual, allowing for more control over the account and its investments.
Choosing the Right Option:
When deciding between an FSA and an HSA, employees should consider their current health insurance plan, medical expenses, and financial goals. If an employee has a high-deductible health plan and wants the flexibility to save for future medical expenses, an HSA might be the better choice. On the other hand, if the employee prefers to use funds within a specific plan year and has a more traditional health insurance plan, an FSA could be more suitable.
Remind your employees that both FSAs and HSAs can provide valuable tax benefits and help them manage their healthcare costs more effectively. Encourage them to review the specific terms, contribution limits, and rules associated with each option before making a decision.
FSAs and HSAs are valuable tools for managing healthcare expenses, each with its own set of advantages and considerations. Understanding the key differences between these two accounts can empower employees to make a well-informed choice that aligns with their financial and medical needs.
Special thank you to Paula Alexander, MA, PHR, SHRM-CP, HR Business Advisor for contributing to this HR Question of the Week.
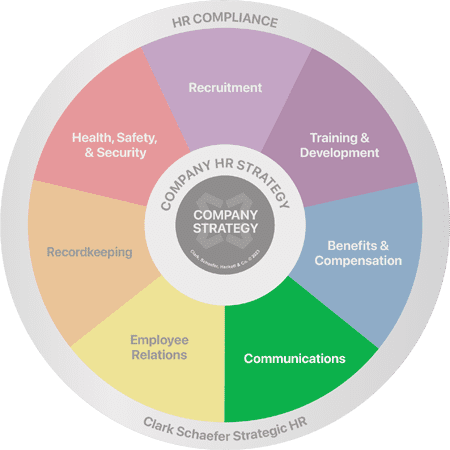
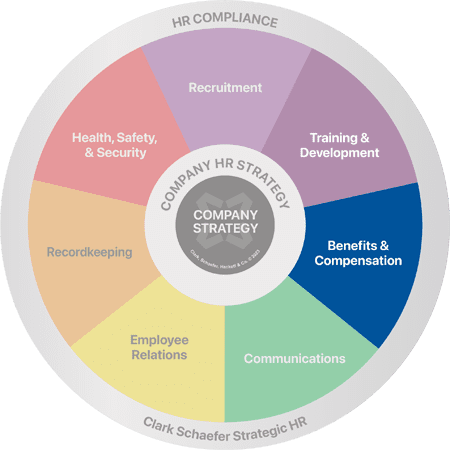
Do you find yourself without answers to tough Benefits and Compensation questions? Whether you need an analysis of your current benefit offerings, a review of your salary structure, or outsourced payroll/benefits administration, Clark Schaefer Strategic HR can do the job. Please visit our Benefits & Compensation page for more information or Contact Us.









 HR Question:
HR Question: