The Opioid Epidemic and Its Cost on Society and the Economy
Last Updated on June 18, 2020 / Health, Safety & Security
Submitted by Signet Screening
How Prescription Painkillers Led to the Opioid Epidemic
The dependence on prescription painkillers and synthetic opioids has exploded into a full-blown epidemic in America. The problem is a 50-state issue that public health officials are calling the worst drug crisis in the American history.
The epidemic’s roots are in chronic pain and what is being looked at as questionable pain management practices. An estimated 25 million adults suffer from daily pain, and another 23 million struggles with severe, recurring pain. The consequences are costly:
- Disability
- Decreased work productivity
- Lower quality of life
- Poor health overall1
Opioids aren’t without a purpose: They’re an effective way to manage pain when prescribed by a physician and taken as indicated. However, the entire class of drugs is highly addictive. When a prescription runs out or is too expensive to maintain, some people may turn to using cheaper street opioids.
The most commonly used opioids are:
- Heroin
- Hydrocodone
- Morphine
- Codeine
In 2014, the U.S. Department of Health and Human Services (HHS) made the epidemic declaration. That year, more people died from drug overdoses than any other year on record with more than six out of ten deaths involving opioids.
Opioids: From the 1970s to now
The history of the crisis is interesting to review and provides perspective on how the situation has gotten to this point.
Throughout the 1970s doctors and nurses were trained to provide minimal opioids for pain, unless death appeared imminent. In the ’80s, a group of prominent pain management specialists began promoting the idea that restraints on prescribing opioids were unnecessary and even cruel.
Kathleen Foley of New York City’s Memorial-Sloan-Kettering Cancer Center wrote two highly influential articles reporting on the low incidence of addictive behavior in small cancer and noncancer patient groups. These articles, and other efforts, started a 20-year campaign for the long-term use of opioids for the treatment of pain in noncancer patients.
Many pain management specialists challenged the idea that chronic opioid therapy was safe, pointing out the risks of addiction, overdose and other side effects. As pain specialists debated these issues, several factors brought opioids to mainstream usage:
- The aggressive marketing of Oxycontin as safe for chronic pain
- The trafficking of cheap, pure heroin in smaller U.S. cities
Purdue Pharma marketed Oxycontin as nonaddictive and safe since it was released within the body over a 12-hour period. However, recreational users learned to use Oxycontin to achieve highs by crushing or dissolving the pills or by taking large doses. Both pill mill operators (unethical doctors who prescribe hundreds of pills without medical justification) and well-intentioned general practitioners wrote a high number of prescriptions for this drug.
The ample supply of Oxycontin made it an attractive option at first, particularly for low-income Medicaid and Medicare patients. But then, addiction and the recurring expense prompted users to find a lower-cost alternative. They began using black-tar heroin (a less expensive form of heroin that’s either sticky like tar or hard like coal), and sellers were readily available to fill the need. Heroin traffickers encouraged use in the West, Midwest and Appalachia by:
- Meeting buyers in safe locations2
- Offering inexpensive product2
- Giving free samples to encourage customer loyalty2
Instead of paying $40 for a pill, Oxycontin users could pay $10 for the same effect. Oxycontin users – including many middle-class teens and young adults – began to see heroin less as a taboo and more of a practical alternative.3
Call-out statistics to use throughout History section
- Overdoses involving prescription opioids and heroin increased 200% between 2000 and 20141
- Drug overdose deaths increased 137% between 2000 and 20141
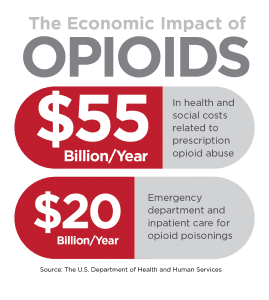
The Social and Economic Impact
As the number of opioid prescriptions grew from 76 million to 219 million between 1991 and 2011, the impact on families, communities and business became devastating. Many experts who initially called for the liberal use of opioids to treat chronic pain began reversing their support due to the alarming reports of abuse and addiction.
The daily statistics are bleak – here’s what happens on an average day in America:
- More than 650,000 opioid prescriptions are dispensed4
- 78 individuals die from an opioid overdose (prescription and heroin)5
- 580 begin using heroin6
- 3,900 begin nonmedical use of prescription opioids6
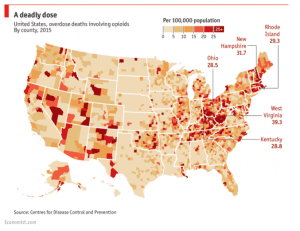
While the number of deaths is highest in major cities, such as Chicago and Baltimore, the greatest overall impact is in Appalachia, New England and the Midwest.
The Epidemic in Ohio
Ohio has been one of the most hard-hit states. The epidemic has strained the resources of law enforcement and the criminal justice and healthcare systems. Ohio’s publicly-funded addiction treatment services are also stretched thin.
The number of drug overdose deaths increased in Ohio by more than 440 percent from 1999 to 2012.7 The Centers for Disease Control (CDC) estimated that unintentional drug overdose deaths cost the state $5.7 million in medical costs and $2 billion in work loss costs in 2012.8
Legislative Efforts
Individual states have tried to crack down on prescription opioid abuse through legislative efforts, setting in-office physician dispensing limits, licensing pain management clinics (pill mills), and establishing patient safety and education programs.
Forty-seven states, including Ohio, Indiana and Kentucky, have established Naloxone Distribution Programs. Naloxone is a drug that reverses heroin’s effects on the brain and jump-starts breathing for overdose victims. The Food and Drug Administration (FDA) approved its use in 1971, and doctors and paramedics routinely have used the drug since then. The distribution programs also provide overdose training and take-home naloxone doses to people considered high risks.
How Is The Opioid Epidemic Affecting Companies?
This epidemic is having negative effects on businesses, as well as within families and communities. Businesses need to take steps to protect their reputation and profitability. Employees with addictions function at about 75 percent productivity, so the direct cost to companies is 25 percent of salaries on that factor alone.
What Can Business Leaders Do?
The first step for business leadership is to review or institute a drug-free workplace program with policies and procedures in place for all employees. A drug-free workplace helps prevent the hiring of illegal substance abuses and helps deter current employees from substance abuse. Business leadership can visit the Institute for a Drug-Free Workplace for more information on establishing a drug- and alcohol-abuse policy.
Companies can also educate and train managers on looking for the signs of addictions and knowing what steps to take if an issue is identified. Signs of potential abuse include:
- Bloodshot eyes and dilated pupils
- Sudden weight loss
- Appearance deterioration
- Mood swings, including displays of aggression and irritability
- Withdrawal from co-workers
- Slurred speech
Companies should also understand the available screening methods for opioids and the capabilities of each method. Many factors – metabolism rate, age, liver and kidney health, and body weight – affect how long opioids can be detected. In general, however, saliva, urine and hair follicle tests can discover the most common opioids after last usage:
| Drug | Saliva Test | Urine Test (most common in employment testing) |
Hair Follicle Test |
| Heroin | 5 hours | 2 to 7 days | Up to 90 days |
| Hydrocodone | 12 to 36 hours | 2 to 4 days | Up to 90 days |
| Morphine | Up to 4 days | Up to 3 days | Up to 90 days |
| Codeine | 1 to 4 days | 1 to 4 days | Up to 90 days |
For current employees, companies are encouraged to support rehabilitation programs for improved recovery rates. Insurance often covers 30-day inpatient programs although much longer treatment periods are needed typically.
Conclusion
The opioid epidemic is taking a toll across America on individuals, families, businesses and communities. Despite efforts, recent data show that the United States is still in the throes of the opioid epidemic. Naloxone programs are preventing a small percentage of overdose deaths, but the rising use of fentanyl – a synthetic opioid painkiller that’s 50 to 100 times more powerful than morphine – is contributing to the situation worsening.
In 2016, fatal overdoses increased 26% in Connecticut, 35% in Delaware and 39% in Maine9. After fatal overdoses soared 62% in the first nine months in 2016, Maryland’s Governor Larry Hogan declared a state of emergency.9
The fight against opioid abuse and its effects will continue for many years. The combined efforts of individuals, community organizations, government legislation and programs, and employers will help the country reverse the abuse of prescription and street opioids.
- Meldrum, ML. The ongoing opioid prescription epidemic: historical context.American Journal of Public Health, 2016:106(8), 1365.
- Quinones, S. Dreamland: The true tale of America’s opiate epidemic.New York, NY: Bloomsbury Press; 2015.
- Mars, SG, Bourgois, P, Karandinos, G, Montero, F, & Ciccarone, D. “Every ‘never’ I ever said came true”: transitions from opioid pills to heroin injecting.International Journal of Drug Policy, 2014;25(2), 257-266.
- IMS Health National Prescription Audit
- CDC National Vital Statistics System
- SAMHSA National Survey on Drug Use and Health
- Ohio Department of Health Office of Vital Statistics
- CDC WISQARS Cost of Injury Reports, based on 2012 Ohio overdose incidents
- Daily chart: America’s opioid epidemic is worsening. http://www.economist.com/blogs/graphicdetail/2017/03/daily-chart-3. March 6, 2017
Thank you to Signet Screening for sharing this article. Their services include federal, state and local criminal checks, education and employment verifications, drug screens, motor vehicle, and social media searches. For more information contact Signet Screening or call 513-330-6695.